Traditional treatment for eating disorders is based upon the assumption that eating disorders are mental illnesses and should be treated with therapy; including individual therapy, family therapy, cognitive behavioural therapy (CBT) and antidepressants medication, such as SSRIs (selective serotonin re-uptake inhibitors). The cause of anorexia nervosa has varied over the last hundred years, ranging from schizophrenia to obsessive-compulsive disorder.
Treatment outcomes with these methods are similar for anorexia nervosa and bulimia nervosa; less than 50% have a good outcome, and half of those who do have a good outcome relapse within a year of completing treatment. A study of CBT and bulimia nervosa demonstrated that four months after treatment 44% of patients had relapsed, and only 14% of the original 194 patients were in remission (Halmi et al. Arch Gen Psychiatry 2002;59:1105).
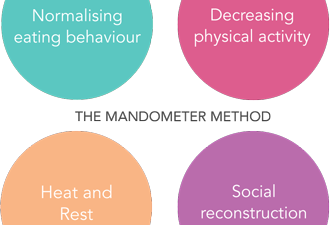
The Mandometer method differs from the conventional approach. We have shown that the psychiatric symptoms, such as anxiety, depression, and obsessive behaviours are consequences of changing eating behaviour, and that these symptoms disappear when eating behaviour and satiety are normalised. Our treatment outcomes are the same, regardless of diagnosis. Approximately 75% of patients go into remission (they are symptom free), and approximately 10% of these patients will relapse during the following five years after treatment.
Learn more about our treatment and results >
The Mandometer method differs from conventional treatment methods.
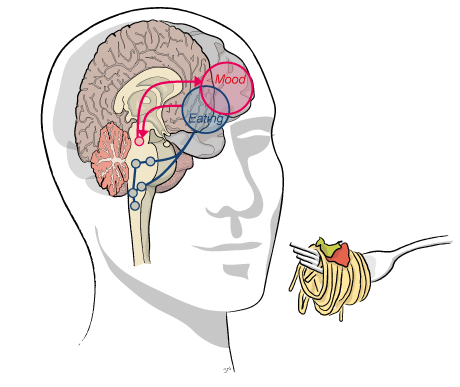
The anxiety, depression and obsessive thoughts that patients experience are not what causes the eating disorder. Instead, these problems are symptoms of starvation and the result of irregular eating habits. As patients regain control over their food intake and eating behaviour normalises, their psychiatric symptoms decrease, and eventually disappear completely.
It is not the fault of the patient, or their parents. Eating disorders are not caused by problems in the family or family relationships. In contrast, problems may arise in the family when a member of the family suffers from an eating disorder.
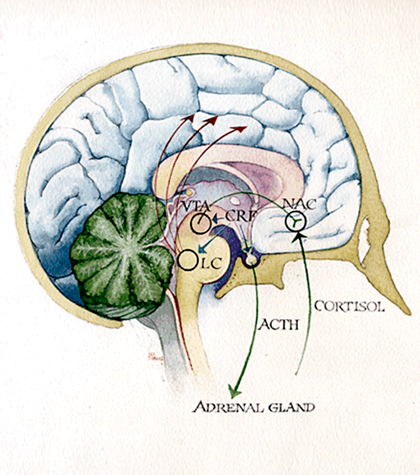
Research shows that antidepressants are not effective in treating the depression associated with eating disorders, and may actually decrease the patient’s appetite, body temperature, learning capacity, and possibly even increase anxiety and suicidal thoughts. If a patient is already taking antidepressants when they commence treatment, our doctors monitor the patient’s condition while gradually reducing the patient’s dose; eventually withdrawing the medication completely. It is important these medications are not withdrawn abruptly; therefore, we reduce the dosage in a controlled manner.
The Mandometer® device that patients learn to eat with teaches them normal eating behaviour and satiety signals. When patients have learned how to correctly identify their biological signals for hunger and satiety, the fear of becoming fat and not being able to stop eating disappears. Only 6% of our patients with anorexia nervosa have developed bulimia nervosa.
It teaches you how fast to eat, how much to eat and when you should eat. Our patients learn that there is no need to exclude any foods in order to maintain a healthy weight, or risk becoming overweight. The Mandometer gives patients a technical tool to control their food intake. They do not need to fear that they are being cheated into eating any more than they should. Learn more about the Mandometer >